TRAM Flap and Physio.
A flap of the woman’s own tissue is used to reconstruct a natural feeling and looking breast. A flap is skin, fat, muscle or any combination of these tissues that is transferred from one part of the woman’s body to another for reconstructive purposes. Common donor sites are the lower abdominal wall and back and less common but useful sites are the buttocks and upper inner thighs.
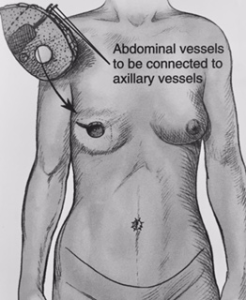
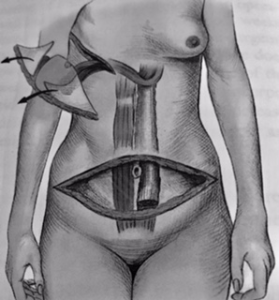
TRAM image 1. Free TRAM Flaps. TRAM image 2. Pedicled Flap transferred while still attached to the abdominal muscle.
Ref: “A Woman’s Decision” free publication via www.synovismicro.com
Free TRAM flap: The fat, skin, blood vessels, and muscle are cut from the wall of the lower abdomen and moved up to the chest to reconstruct the breast. The surgeon reattaches the blood vessels of the flap to blood vessels in the chest using microsurgery. In the “muscle-sparing” free TRAM flap the surgeon uses a smaller part of the rectus abdominis muscle for the flap, instead of a large portion of the muscle, lowering the risk of losing abdominal muscle strength.
A pedicled (or attached) TRAM flap: Now the fat, skin, blood vessels, and muscle from the lower abdominal wall are moved under the skin up to the mastectomy site to rebuild the breast. The blood vessels (the artery and vein are the pedicle) of the flap are left attached to their original blood supply in your abdomen. Pedicled TRAM flaps use a large portion of the rectus abdominis muscle and are known as “muscle-transfer” flaps. Recovery is longer and the risk of losing abdominal muscle strength is higher.
TRAM Outcomes
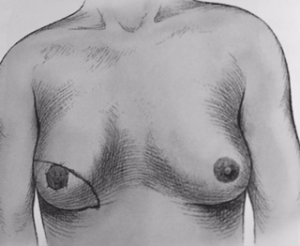
Tram flaps look and feel natural and soften and drop like the other breast over the next several months. Over time the reconstructed breast also ages like the other breast. The other breast may also get a surgical lift to achieve symmetry. While the patient does have a new and lengthy abdominal scar the “tummy tuck” is generally appreciated.
TRAM physio guidelines: The transverse rectus abdominis muscle stabilizes the abdominal oblique muscles and so resecting it results in abdominal wall and core weakness. The ability of TRAM patients to recruit the abdominal muscles is permanently compromised. A history of low back problems contraindicates a TRAM as it contributes to less spinal support and stability.
For 4-8 weeks post-op these patients are unable to stand upright and will benefit from learning spinal precautions during activities of daily living (ADLs) e.g. rolling onto their side when transferring from supine to standing, using their hips and knees when lifting, driving and doing ADLs that involve forward flexion. Housework e.g. making beds, filling the dish washer, lifting food in and out of the low oven and vacuuming are particularly difficult to do. Spinal precautions will help TRAM patients do the ADSLs while also avoiding straining the surgical sites and their lower backs.
The abdominal wall becomes permanently numb due to nerve disruption when creating the tunnel, so observe skin precautions if using ice and hot packs.
Arm motion is limited and abduction is discouraged in the early weeks. Patients can begin gentle shoulder range of motion (ROM) 2-3 weeks post-operatively and begin abdominal exercises 2 months post-op. As with all major abdominal surgery, lifting and driving is avoided for 2 months and after that started carefully.
Because trunk flexion is permanently impaired, patients cannot do “100s” in Pilates, and are advised to rebuild core strength slowly and carefully, advancing from level one only if and when they can maintain the pelvis in a neutral position. Teaching and observing pelvic neutral is a key step in early breast cancer reconstruction rehab.
TRAM Image 3. Final TRAM scar and reconstructed and tattooed nipple-areola.
Contact Siobhan@theoreillycentre.ie with your comments and questions.